Understanding the Connection Between Early Menstruation and Cervical Cancer
Cervical cancer has a multifaceted relationship with early menstruation (menarche), highlighting how reproductive and hormonal factors can influence long-term health. While cervical cancer is primarily caused by persistent HPV infections, the age at which menstruation begins can amplify the risk through various biological, social, and cultural factors. This article unpacks the connection between early menarche and cervical cancer, exploring how prolonged hormonal exposure, early sexual maturity, and harmful cultural practices may increase vulnerability. By understanding these dynamics, we can better emphasize preventive strategies like HPV vaccination, education, and regular screenings to protect women’s health.
AHUMUZA MARTHA NYAKATO - Medical Student
1/21/20254 min read
Understanding the Connection Between Early Menstruation and Cervical Cancer
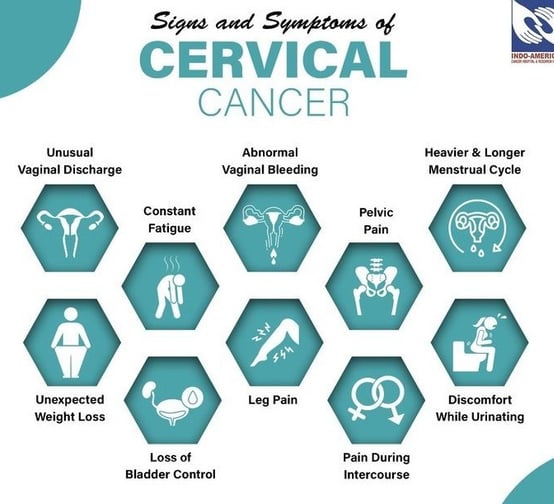
Cervical cancer is a type of cancer that begins in the cells of the cervix, the lower part of the uterus that connects to the vagina. It is one of the most preventable cancers due to early detection methods like Pap smears and HPV vaccines. Despite this, it remains a leading cause of cancer-related deaths among women worldwide, especially in developing countries. Cervical cancer is often caused by a persistent infection with certain strains of the human papillomavirus (HPV). However, other risk factors, including lifestyle and reproductive history, can also influence its development.
One such factor that has drawn attention is the age at which a girl starts her menstrual periods (menarche). Research suggests that starting menstruation at an early age may increase the risk of cervical cancer later in life. This article explores this connection, its underlying reasons, and what it means for women’s health.
Why Early Menstruation May Be Linked to Cervical Cancer
The relationship between early menarche and cervical cancer risk is complex and influenced by multiple factors. Here are the key insights:
1. Longer Exposure to Estrogen
Starting menstruation early means a longer reproductive life span, during which a woman’s body is exposed to estrogen and progesterone. Estrogen, in particular, can influence the growth and behavior of cervical cells, potentially making them more susceptible to HPV infection or other changes that lead to cancer over time.
2. Increased Lifetime Risk of HPV Infection
Early menstruation often signals the start of hormonal and physical changes that lead to sexual maturity. Girls who start their periods earlier may begin sexual activity earlier, whether due to societal norms, cultural practices, or biological readiness. This increases the likelihood of exposure to HPV, the primary cause of cervical cancer, over their lifetime.
In some communities, harmful cultural practices further amplify this risk. For instance, in certain tribes, there is a tradition where girls are raped or forced into sexual initiation by an older man as a rite of passage into adulthood upon starting their menses. This practice not only violates the rights and dignity of young girls but also exposes them to sexually transmitted infections (STIs), including HPV. These practices significantly increase the risk of cervical cancer later in life due to early and often unprotected exposure to the virus.
Such traditions underscore the urgent need for education, advocacy, and legal reforms to protect young girls from harmful cultural practices and to promote safe, healthy transitions into adulthood. Addressing these issues is not only a matter of public health but also a critical step toward safeguarding the human rights of vulnerable populations.
https://www.bbc.com/news/magazine-36843769
3. Cervical Vulnerability During Adolescence
The cervix undergoes significant changes during puberty. During this time, the cells of the cervix are particularly vulnerable to damage and infection, including HPV. Early menarche extends this vulnerable period, increasing the chances of cervical abnormalities that can develop into cancer later.
4. Indirect Links to Lifestyle Factors
Early menarche is sometimes associated with factors like obesity, poor diet, or low socioeconomic status, which can independently increase the risk of cervical cancer. These conditions may limit access to preventive healthcare, such as HPV vaccination and regular cervical screening.
What Does Research Say?
Numerous studies have investigated the connection between early menarche and cervical cancer. For example:
A 2017 meta-analysis found that women who began menstruating before the age of 12 were slightly more likely to develop cervical cancer compared to those who started later.
Research also highlights that early menarche may overlap with other risk factors, such as early onset of sexual activity, multiple pregnancies, and inconsistent use of barrier contraceptives.
While early menarche alone doesn’t directly cause cervical cancer, it can amplify the effects of other risk factors, making prevention and early intervention crucial.
Prevention Strategies
Understanding the risks associated with early menarche can empower individuals and communities to take preventive measures against cervical cancer:
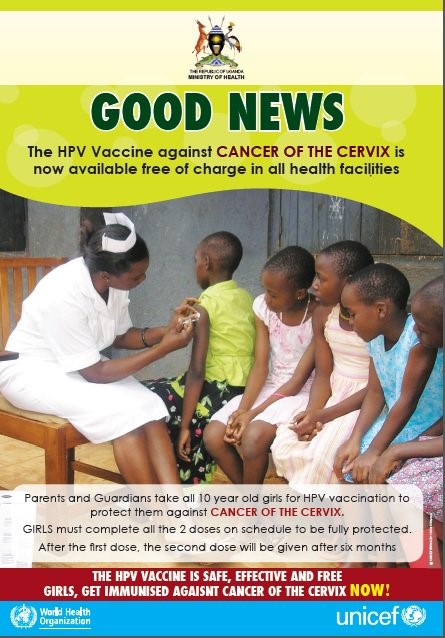
1. HPV Vaccination
The HPV vaccine protects against the strains of HPV most commonly linked to cervical cancer. It is most effective when given before a girl becomes sexually active, typically between the ages of 9 and 14
Although people above said age can receive the vaccine it might be less effective if they’ve engaged in sexual intercourse as they might already have the human papilloma virus(HPV) hence making the vaccine not as effective.
2. Regular Screening
Pap smears and HPV tests can detect abnormal cervical changes early, when they are most treatable. Women should begin screening at age 21 and follow their healthcare provider’s recommendations for frequency.
3. Healthy Lifestyle
Maintaining a balanced diet, staying physically active, and avoiding smoking can improve overall health and reduce the risk of cancer.
4. Education and Awareness
Teaching young girls and their families about the importance of reproductive health, safe sexual practices, and the risks of HPV can help them make informed decisions.
Conclusion
While early menarche may slightly increase the risk of cervical cancer, it is just one piece of a larger puzzle involving genetics, lifestyle, and healthcare access. By prioritizing prevention through HPV vaccination, regular screening, and education, women can significantly reduce their risk. Cervical cancer is one of the few cancers that is largely preventable, and understanding the factors that contribute to its development is a vital step toward eradicating it.
Every woman deserves access to the tools and knowledge necessary to protect her health. By fostering awareness and taking proactive steps, we can ensure a brighter, healthier future for generations to come.
Written by;
AHUMUZA MARTHA NYAKATO
Med student


Empowering women and girls through advocacy for menstrual equity
Support
Advocacy
© periodtalkuganda2025 . All rights reserved.
+256762900000
